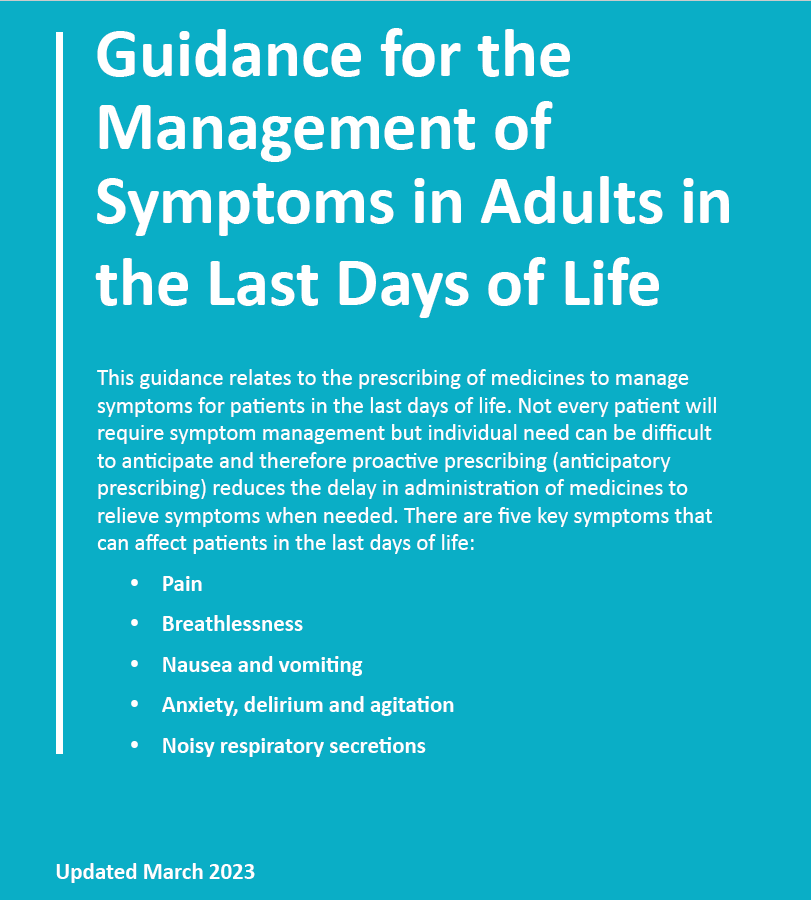
The guidance recognises the dying person may be unable to tolerate oral medicines. Therefore, administration is via the subcutaneous (SC) route (SC injection and SC syringe pump over 24 hours).
When it is recognised that a person may be entering the last days of life:
Users are advised to:
|
Details of Palliative Care Network Pharmacies and Palliative Care Supply Service pharmacies (i.e. those with extended opening hours who are contracted to stock the regional palliative care medicines list) can be found at Palliative Care (hscni.net) https://hscbusiness.hscni.net/services/2481.htm
Further information is available from your Specialist Palliative Care Team, the Palliative Adult Network Guidelines (PANG) Book 2016 and at www.book.pallcare.info
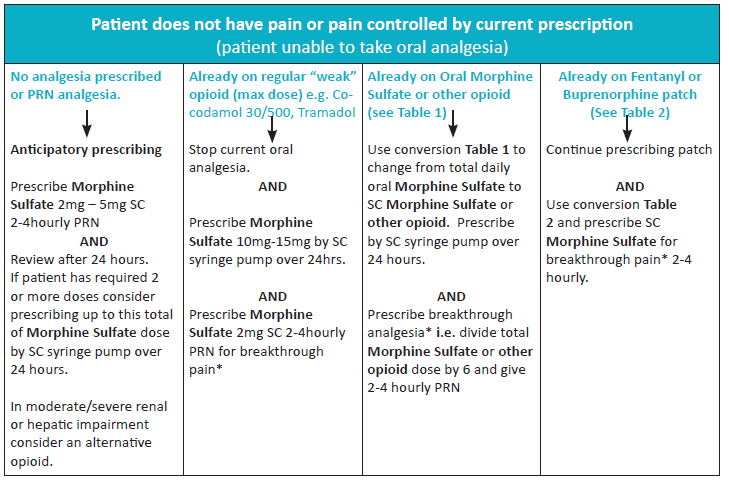
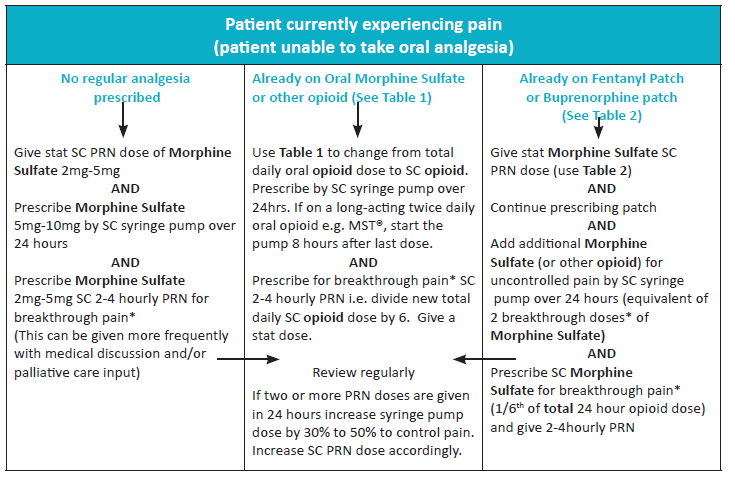
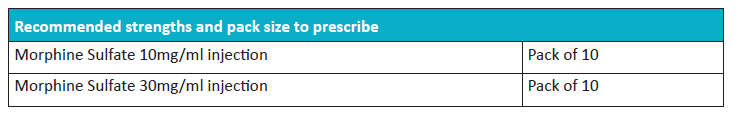
Pain
Morphine Sulfate is the 1st line choice of strong opioid in non-specialist settings. Renal failure is an exception – see choice of 1st opioid with renal impairment section below.
Opioid Conversions Tables
- Refer also to HSC Guidance “Northern Ireland guidelines on converting doses of opioid analgesics for adult use”.
- Morphine Sulfate is the first line choice of strong opioid in non-specialist settings. Renal failure is an exception- see choice of 1st opioid with renal impairment section below.

Example Opioid Calculations
Changing from Oral Morphine to SC Morphine via syringe pump.
1. Work out total oral dose Morphine in 24 hours
e.g. MST 15mg BD = 30mg morphine total/ 24 hrs
2. Convert from oral to SC route
e.g. 30 ÷ 2 = 15mg Morphine SC syringe pump over 24hours
And
Calculating the oral breakthrough/ PRN dose (immediate release preparation)
1. Work out total oral dose Morphine in 24 hours
e.g MST 15mg BD = 30mg total/24hours
2. Divide by 6 to get 1/6th of the dose
e.g. 30 ÷ 6 = 5mg Morphine Sulfate Oral Solution (Oramorph®) PRN 2 to 4 hourly
And
Calculating the SC breakthrough/ PRN dose
Divide total SC morphine dose in 24h by 6
e.g. Morphine 15mg via syringe pump over 24h = 15 ÷6 = 2.5mg. Prescribe 2mg Morphine Sulfate injection SC PRN 2 to 4 hourly. For safety and clarity, prescribe in whole milligrams. Use of decimal places should be avoided.
Note: Breakthrough analgesia is usually worked out as 1/6th of the total 24 hour opioid dose, but can also be given as 1/10th of the total 24 hour opioid dose. Refer to BNF “Prescribing in Palliative Care” section.
Choice of first opioid with renal impairment
|
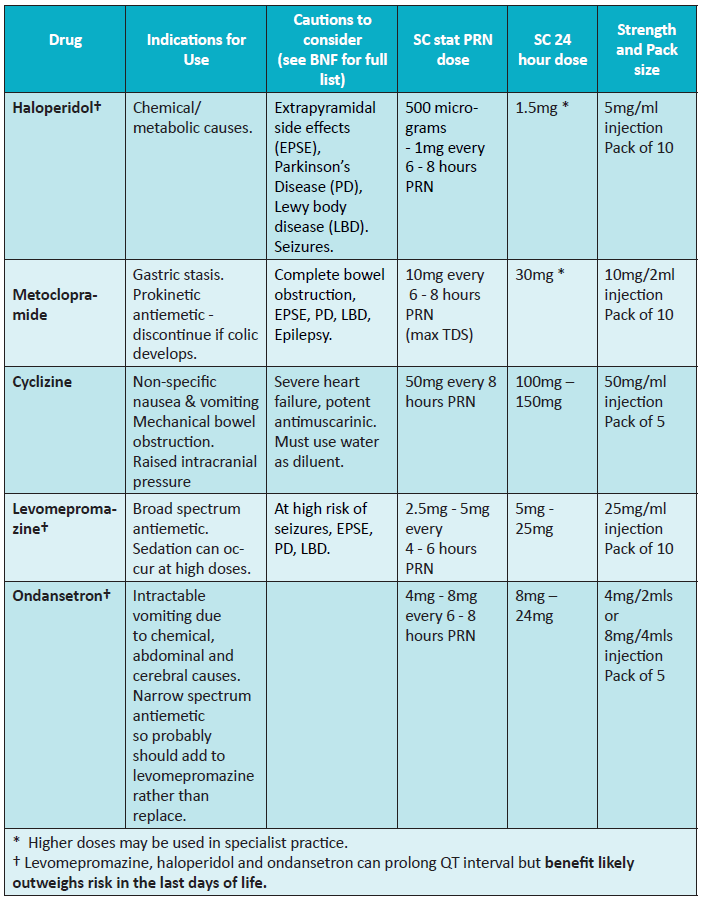
Nausea and Vomiting
Consider potentially reversible causes such as constipation, hypercalcaemia, infection and raised intracranial pressure. Choice of antiemetic should be influenced by likely underlying causes.

Table 3. Choice of Antiemetic
Lower doses are indicated in severe renal or hepatic impairment
Breathlessness
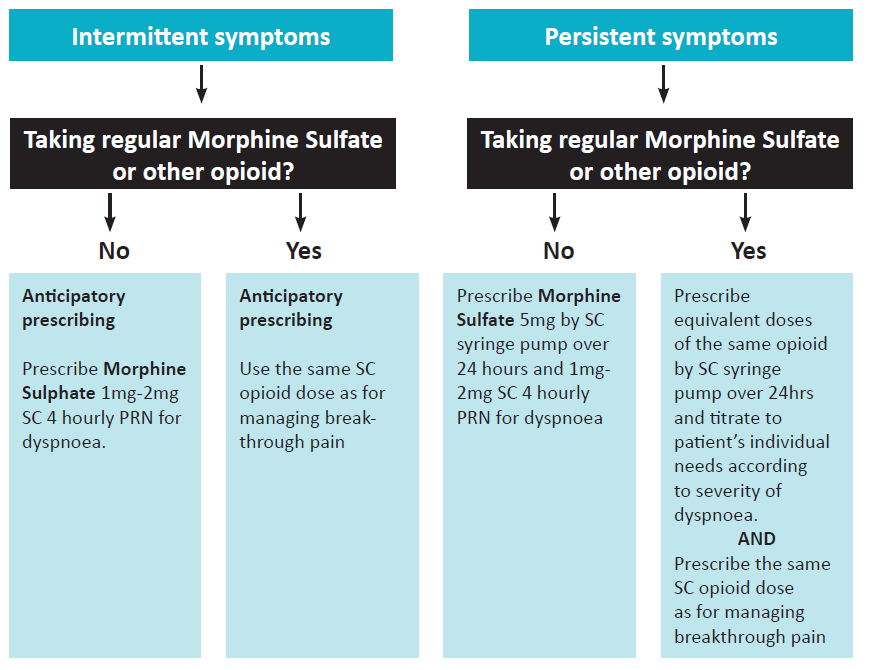
For patients on other opioids use Table 1 for opioid conversions and use guidance as above
- For patients who are conscious and can tolerate oral medicines consider oral opioid in a dose equivalent to the SC doses recommended above.
- Oxygen is only indicated for patients who are are hypoxic.
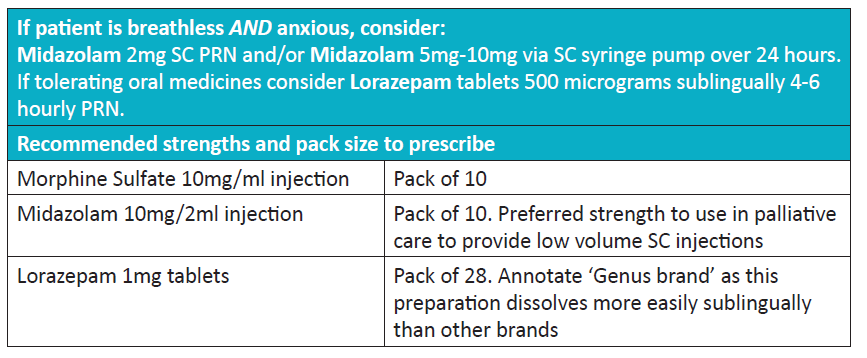
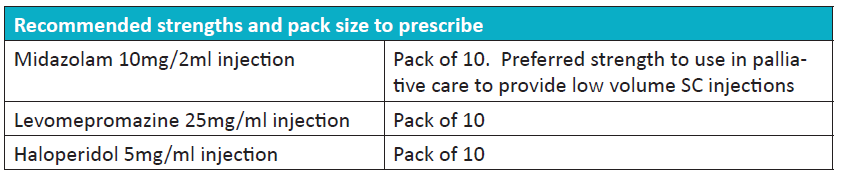
Anxiety, Delirium and Agitation
Assess the patient first to exclude potentially reversible and treatable causes such as pain, drug withdrawal including nicotine, urinary retention or severe constipation.

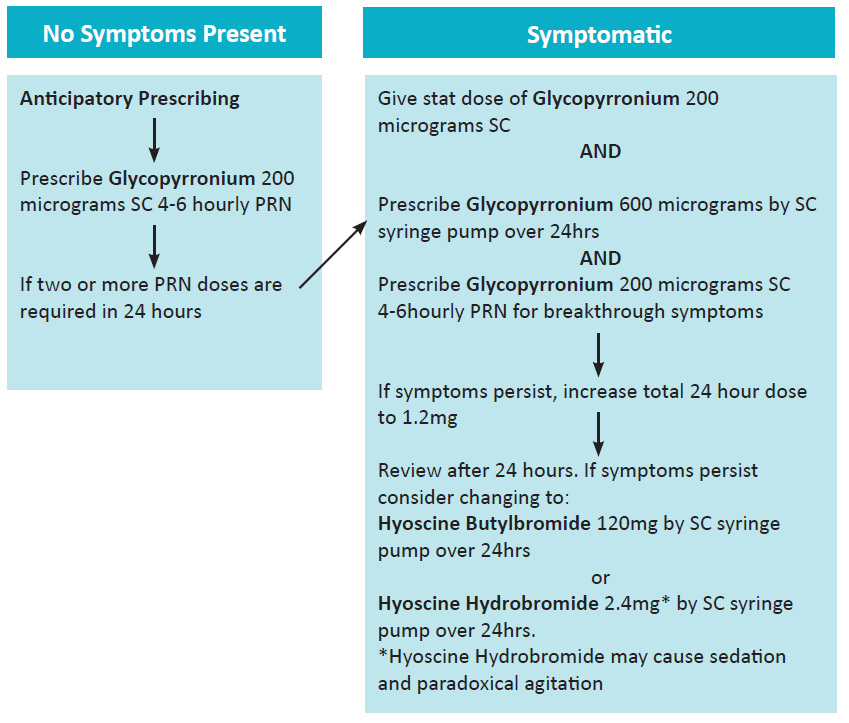
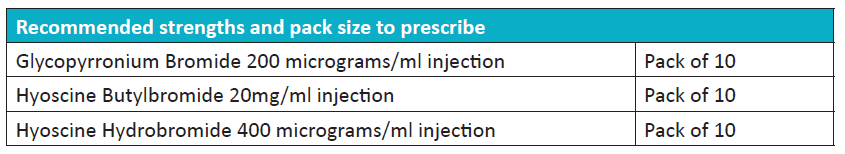
Noisy Respiratory Secretions
- Repositioning can be Early use of anti-secretory agents should be considered and can prevent accumulation of new secretions, although has limited effect in clearing those already accumulated.
- Reassure family and carers that although respiratory secretions sound uncomfortable, if the patient is deeply asleep or unconscious, they are most likely not distressed by them. They are present because the patient is not coughing or clearing their throat as they normally would.
- Good mouth care is essential in reducing the sensation of thirst. Use of intravenous or subcutaneous fluids should be reviewed as part of the patient’s individualised care plan.