End of Life Care in Care Homes during the Covid-19 Pandemic
It is recognised that people living in care homes are often frail with complex needs and varying levels of dependence. Around 80% of people living in care homes are likely to be in their last year of life[1].
Many of those living in care homes will be at greater risk if they were to contract COVID-19 due to conditions such as frailty, cognitive impairment including dementia, physical disability, neurological conditions and multiple comorbidities. For many, hospital admission during the pandemic may be inappropriate which means additional support within the care home setting may be necessary, more comfortable and in the best interests of those in the last days of life.
Evidence is increasingly indicating that, in the care home and older populations, the two most well-known/common COVID-19 symptoms are not the only presenting symptoms. More information regarding symptom checking in nursing and residential care homes can be found at the link below:
The following information has been compiled by the Palliative Care in Partnership (PCiP) Programme, as an overview of mechanisms and resources in place in Northern Ireland to support care homes caring for people in the last days of life during the Covid-19 pandemic:
Covid-19: Management of Symptoms in the Last Days of Life (RPMG April 2020)
The Regional Palliative Medicines Group (RPMG) working with the NI Specialist Palliative Care Pharmacy Group and supported by the PCiP programme have developed specific symptom management guidance for people with Covid-19 in the last days of life. This guidance (link below) is relevant for use in both secondary and primary care settings (including care homes).
Covid- 19: Management of Symptoms in the last days of life (RPMG April 2020)
[1] Royal College of Physicians: Talking about dying: How to begin honest conversations about what lies ahead. October 2018.
Regional arrangements for palliative care medicines during Covid-19 pandemic
In response to the COVID-19 pandemic, the Health and Social Care Board (HSCB) has been working to support the availability of essential medicines for palliative/end of life patients who are managed in primary care settings, including care homes.
Community Pharmacy Palliative Care Network
Community Pharmacy Palliative Care Network pharmacies are spread throughout Northern Ireland and aim to increase access to community pharmacy palliative care services. They can supply medicines from the palliative stock list or be contacted for advice. Please see the leaflet below for more information.
Community Pharmacy Palliative Care Network (including regional palliative stock list)
More information about Palliative Care Pharmacy Services can be accessed here: http://www.hscbusiness.hscni.net/services/2481.htm
Urgent Pandemic Packs for Nursing Homes
HSCB has also arranged the distribution of Urgent Pandemic Packs to Nursing Homes with 59 beds or more. The medication in these packs should be used to provide timely access to patients requiring clinically urgent medication and guidance to support the use of these packs will be issued to eligible nursing homes prior to delivery.
On 1st May 2020, HSCB issued a communication about the further supply of urgent pandemic packs to nursing homes in Northern Ireland to advise on a further phased roll out to Nursing Homes who have not yet received an Urgent Pandemic Pack. Distribution of packs was further rolled out and offered to all Nursing Homes across NI registered with RQIA. Distribution now complete with 96% homes having packs in place.
For more information on the Urgent Pandemic Packs and a list of the Nursing Homes who will receive them please visit the link below:
http://www.hscbusiness.hscni.net/services/3162.htm
Advance Care Planning
Ideally all people living in care homes should already have documented Advance Care Planning Summaries. Further information regarding advance care planning and using the ‘Your Life, Your Choices – Plan ahead’ resources can be found in the resources section of the Palliative Care in Partnership website https://pcip.hscni.net/resources/
If advance care planning discussions and decisions have already taken place with regards to the care preferences of the person then those decisions should be reviewed and confirmed (or changed) in light of Covid-19 with person/ those important to them (if the person lacks capacity).
The nature of Covid-19 presents a risk to all people living in care homes even those which are currently considered stable. Anticipatory plans in case of the person becoming infected should be discussed with and for each person to establish clear understanding of goals of care. These discussions may include:
- Use of IV/SC fluids
- Use of oxygen or antibiotics (if appropriate)
- When/if to transfer the person to hospital
- DNACPR and/or ADRT
- Their wishes for the last days of life
All discussions should be clearly documented and if necessary involve the person’s GP who can document agreed decisions relating to medical interventions and share these via the patient’s Key Information Summary (on NIECR) so that they are available to colleagues in other care settings.
In the event that the person is admitted to hospital (or another care setting) for treatment the care home should ensure that details of their advance care planning preferences are transferred with the person.
Having difficult conversations
The Scottish Quality Safety Fellows – NHS Scotland have developed a ‘roadmap’ to support health care professionals who may not be routinely used to discussing end of life decisions, death and dying with people or those important to them. Please see Appendix 1 for more information.
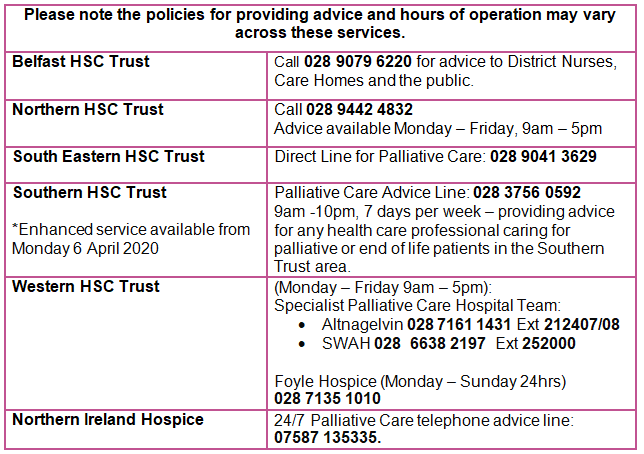
Support from palliative care professionals
The existing Specialist Palliative Care services offered by each HSC Trust and the local hospices across Northern Ireland will continue to operate, although some face to face services may be restricted in line with Government advice and social distancing measures.
Some of these providers are also enhancing their services to offer additional telephone advice to health professionals (including care home staff) caring for people in their last days of life.
Verification of Life Extinct
It is recognised that during the Covid-19 pandemic there is a need to increase the number of people appropriately trained to verify life extinct. Increased capacity in appropriately trained staff who can verify life extinct will relieve pressures on medical practitioners particularly in community settings.
Through RQIA, the Chief Medical Officer and Chief Nursing Officer have written to all independent care providers (including nursing and residential homes) requesting that providers encourage nurses to access free on-line training which is being offered by the HSC Clinical Education Centre. For more information please visit https://cec.hscni.net/ and search for ‘Verification of Death’ under ‘Programmes’.
In addition, an outline ‘Verification of Life Extinct (VLE) in a Nursing or Residential Care Home Policy’ has been drafted and is available to Care Home Providers as a template to provide core elements from which you can develop your own policy and a series of Frequently Asked Questions is also available.
Covid-19 Guidance surrounding death
A range of guidance surrounding deaths in Northern Ireland during Covid-19 has been developed and is available on the Department of Health website at the link below:
https://www.health-ni.gov.uk/publications/covid-19-guidance-surrounding-death
This guidance includes new arrangements for completing and issuing Medical Certificates of Cause of Death and guidance for verification of life extinct during Covid-19.
Death and Grieving in Care Homes
Death and grieving in a care home during the Covid-19 pandemic has been developed as a guide to support care home staff, residents and their families during these unprecedented times. This guidance has been written by Dr Frances Duffy, Consultant Clinical Psychologist, Northern Health and Social Care Trust in collaboration with the British Psychological Society Faculty of the Psychology of Older People and the Public Health Agency
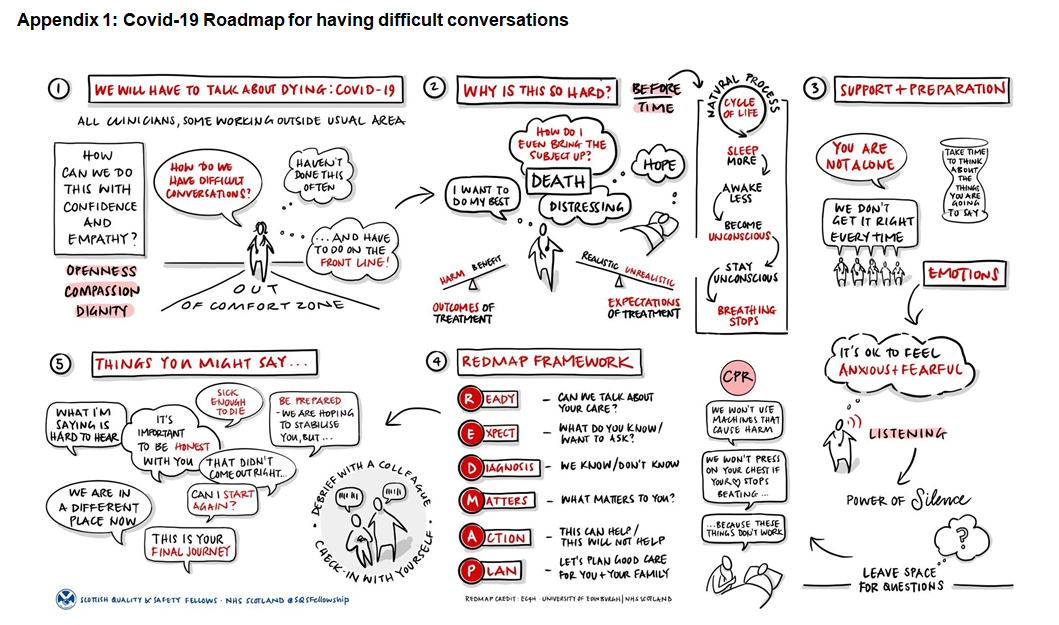
Download – Covid-19 Roadmap for having difficult conversations
